- Clinically proven weight loss
- Daily injections
- Suitable for high BMI patients
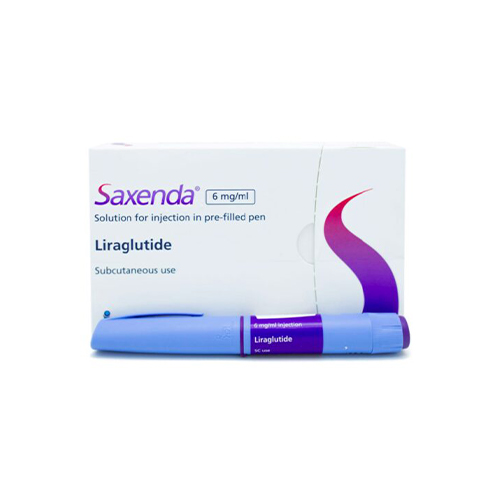
Saxenda Injections
Saxenda Injections are a weight loss medicine sometimes known as “the skinny pen”, contains the active substance liraglutide. It works by acting on receptors in the brain that control your appetite, causing you to feel fuller and less hungry.
What are Saxenda Injections?
Saxenda is a treatment for weight reduction. It is produced by the Pharmaceutical company Novo Nordisk. Saxenda is a Prescription Only Medication (POM), which means it can only be prescribed by a doctor or a prescribing Health Care Professional. Saxenda is often referred to as the “Skinny Jab”.
Saxenda is formulated as an injection pen. It works by suppressing appetite and also provides better glycaemic (blood sugar level) regulation when compared to other medicines that are sold for weight loss.
It is suggested for use in obese patients with a BMI (Body Mass Index) of more than 30. It can also be used in patients with a BMI of 27 or more if they already have at least one weight-related comorbid disorder such as diabetes or high blood pressure.
Saxenda is scientifically proven to help with weight loss, with some studies showing around 1 in 3 patients reporting a 10% or more weight loss after completing a treatment course.
How does it work?
Saxenda contains the active ingredient ‘liraglutide’ which is a synthetic form of GLP-1 (Glp 1 Receptor Agonist) hormone found naturally in the human body.
GLP-1 controls the consumption of food and calories. Through binding the GLP-1 receptor and stimulating it, Saxenda therefore helps control your appetite, ensuring you consume smaller meals, less often.
How to use Saxenda Injections
Saxenda can be used once a day with or without food.
It is available as a pre-filled pen that will require additional disposable screw-on needles each time it is administered.
It is a shallow needle that is injected just beneath the skin in the space known as the subcutaneous compartment. It should be injected into the thigh or upper arm at around the same time every day. After each use, the injection needle should be removed. Always store the pen without a needle to prevent future infections. Never share this product or the needle with others.
Saxenda should only be administered beneath the skin (subcutaneously) and should not be injected intravenously or intramuscularly.
How long does it take to start working?
Saxenda is a once-daily injection. Peak blood levels are typically seen between 10-12 hours after administration.
Weight loss can often be noticed as early as a few days after starting the treatment, to maximise the benefits of Saxenda, it is important to combine this with other weight management strategies such as dietary modifications and exercise.
How long can I safely use Saxenda for?
Saxenda needs to be used alongside regular exercise and a calorie-controlled, balanced diet in order to achieve the best results. The product guidelines recommend that if the patient has not lost a minimum of 5% of their initial body weight within the first 12-weeks after starting on Saxenda, the treatment should be stopped, and alternative weight-loss treatments explored at the stage. If however, at least 5% of the weight is lost, then the product is licensed to be used for up to 3-years or until the BMI reaches a minimum of 23, whichever is first.
Saxenda should also be stopped once the patient has reached a good (satisfactory) weight.
How long does the Saxenda pen last?
The initial dose in the first week is 0.6 mg, and if tolerated, it is then increased gradually every other week by 0.6 mg until a dose of 3 mg is reached. Therefore, the duration of time that 1-pen lasts, will initially change depending on the daily dosage.
If you inject 3 mg of Saxenda daily, each pen will last for 6 days.
How should Saxenda be stored?
Unopened pens should be stored in a fridge (2 °C-8 °C). Once opened, it can be left out of the fridge for up to 30-days.
Saxenda should not be used if the solution has been frozen at some time, so should not be kept at the back of the fridge where it is more likely to freeze, or stored in a freezer.
Side effects & precautions
Before you start using Saxenda, it’s important to make sure that it’s right for you. You should note that Saxenda is contraindicated (not suitable) for the following:
- Patients with a personal or family history of medullary thyroid carcinoma (MTC ) and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2)
- Patients with a prior serious hypersensitivity reaction to liraglutide or to any of the product components
- Pregnant women
Saxenda and Victoza® both contain the same active ingredient, liraglutide, and therefore should not be used together. Saxenda should not be used in combination with any other GLP-1 receptor agonist.
Saxenda has not been studied in patients taking insulin. Saxenda and insulin should not be used together, or in patients using insulin to treat diabetes.
The safety and efficacy of Saxenda in combination with other products for weight loss, including prescription drugs, over-the-counter drugs and herbal preparations, have not been established. Consult your doctor if you are taking any such treatments.
Common side effects
There are a number of side effects of Saxenda. The most common include:
- Nausea
- Diarrhoea
- Constipation
- Headache
- Vomiting
At the beginning of treatment, nausea, headaches and constipation/diarrhoea are more commonly seen, but these side effects generally improve as the body adapts to the treatment. Local skin reactions at the site of the injection are also typically seen.
Serious side effects
As part of your saxenda weight loss journey, it’s possible to experience some serious side effects of this treatment.
In laboratory studies on mice, Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumours (thyroid cancer) at clinically relevant exposures. It is unknown whether this is replicated in humans (thyroid C-cell tumours, including medullary thyroid carcinoma).
- Symptoms of thyroid tumours (tumors):
- mass in the neck
- dysphagia (difficulty/pain swallowing food)
- dyspnoea (shortness of breath)
- persistent hoarseness.
If you notice these symptoms, immediately request medical consultation with your doctor.
Acute pancreatitis has been observed in patients treated with liraglutide.
Symptoms of pancreatitis:
- Persistent severe abdominal pain (can radiate to back)
- Nausea
- Vomiting
Other serious side effects
If you notice these symptoms, immediately request medical consultation.
- Saxenda may cause gallbladder problems, including gallstones.
- Heart Rate Increase (tachycardia)
- Acute renal failure and worsening of chronic renal failure
- Serious hypersensitivity reactions (eg, anaphylaxis and angioedema) have been reported in patients treated with liraglutide.
- Suicidal Behaviour
- low blood sugar (hypoglycaemia) in people with type 2 diabetes who also take medicines to treat type 2 diabetes.
FAQs
Does Saxenda work for weight loss?
The manufacturers of Saxenda (Novo Nordisk) claim that almost 85% of people who start using this medication notice a reduction in body weight within 12 weeks.
Around 60% of people notice at least a 5% reduction in body weight, and 1 in 3 people using Saxenda noticed significant weight loss of more than 10% of their starting body weight in the first 3-4 months.
In a clinical study of people taking Saxenda for 3 years, 56% achieved significant weight loss at year 1. Approximately half of these patients maintained weight loss at 3 years when taking this medication added to a reduced-calorie meal plan and increased physical activity, compared with people not on the drug.
What needles can be used with Saxenda?
The manufacturers of Saxenda claim that almost 85% of people notice a reduction in body weight within 12 weeks.
Around 60% of people notice at least a 5% reduction in body weight, and 1 in 3 people using these weight loss injections noticed significant weight loss of more than 10% of their starting body weight in the first 3 to 4 months.
How much weight can you lose on Saxenda?
The manufacturers of Saxenda claim that almost 85% of people who start using Saxenda, notice a reduction in body weight within 12-weeks.
Around 60% of people notice at least a 5% reduction in body weight, and 1 in 3 people using Saxenda noticed significant weight loss of more then 10% of their starting body weight in the first 3-4 months.
What happens if you eat too much on Saxenda?
Saxenda works by suppressing appetite as well as increasing the feeling of fullness after smaller meals. Most people find they eat significantly less than they would normally prior to starting this medication.
Can you drink alcohol on Saxenda?
We recommend that you reduce the amount of alcohol ingested during the use of Saxenda, as alcohol can increase the risk of prolonged low blood sugar, which can sometimes be dangerous.
Can I just stop taking Saxenda?
If you do not tolerate Saxenda or do not achieve the recommended minimum weight loss of 5% within 12 weeks of starting, you need to stop using it. Even if you are successful at losing weight, and you reach your weight loss goals, treatment can be stopped immediately.
Do you gain weight after stopping Saxenda?
Upon discontinuation, it is likely that you may gain weight, however, studies have shown that the rate of weight gain after stopping, in patients using Saxenda was less than those who lost weight with diet and exercise alone.
How do I inject Saxenda?
Inject your dose under the skin (this is called subcutaneous injection) in your stomach area (abdomen), upper leg (thigh), or upper arm as instructed by your healthcare provider. Do not inject into a vein or muscle. Please see the instructions for use for more information
What if Saxenda is not refrigerated?
Store new, unused Saxenda pens in the refrigerator between 36°F and 46°F (2°C to 8°C). After first use, store in a refrigerator or at room temperature between 59°F and 86°F (15°C to 30°C). Pens in use should be thrown away after 30 days even if they still have medication left in them. Don’t freeze Saxenda. If frozen, it must not be used.
Treatment duration
Studies have shown the safe use of Saxenda for more than three years.
Are there special Saxenda meal plans?
For those prescribed Saxenda, Access Doctor recommends SaxendaCare support to help you make healthy food choices and be physically active. This support helps you focus on making small changes, identify hunger triggers and optimise environmental challenges in weight loss. Visit SaxendaCare to get started.
Can you take more than 3mg of Saxenda?
It is not recommended to use more than the maximum daily dose of 3mg.
Can I take Saxenda with other weight loss drugs?
Saxenda has not been evaluated in combination with other prescription weight-loss medicines or weight-loss supplements. It has the potential to change how other medicines are absorbed. Use caution when taking Saxenda with oral medicines. Tell your healthcare provider about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
What physical activity do you recommend?
You’ll work with our healthcare professionals (weight loss experts) to follow a low-calorie meal plan and increase your physical activity while taking this medication for weight management.
How long does Saxenda take to work?
Saxenda works by acting on receptors in the brain that control your appetite, causing you to feel fuller and less hungry. This will help you eat less food and therefore reduce your weight. Weight loss normally starts within 2 weeks and continues for 9 to 12 months.
What happens if my Saxenda pen stops working?
If you notice that your Saxenda pen is not working anymore, it’s important that you make sure it’s set up correctly and that you know how to use it properly to administer the treatment.
You should refer to the instructions for use which accompany the pen for full instructions. However, here are some quick tips on how to ensure your pen works as it should.
- Check the medication to ensure it’s the correct type, making sure it is clear and colourless
- Attach a new needle each time you need to use your pen
- Before use, check the flow of the pen by turning up the dose selector until it shows the flow check symbol. Then press the dose button until the counter returns to 0.
- Use the dose counter on the pen to view and centre the appropriate dosage before use
- Refer to the dose pointer to ensure the arrow is in line with your selected dose amount
- Turn the dose selector to achieve the correct dosage
- Press down on the dose button to inject into the skin, holding the pen down until the dose counter shows 0. This should be around 6 seconds
- Always replace the pen cap after use to protect the medicine from light
How do I dispose of my Saxenda pen?
Place the needle, or pen with a needle attached, in a sharps disposal container. Do not recycle the needle or pen. Take your sharps bin to a collection site or your local pharmacy.
What needles can be used with Saxenda?
We recommend 6mm 31G needles. These can be purchased separately. They come with a free sharps bin.
How long does a Saxenda pen last?
Once you are taking the maximum dose of 3mg daily, each pen will last 6 days.
Documentation
Saxenda Patient Information Leaflet (PIL)


We’re here to help.
Our friendly team is available to help Monday to Friday 9:00am - 5:00pm.
If you need urgent assistance, do not use this service. Call 111, or in an emergency call 999.