Showing 12 products
Pagination
What is asthma?
Asthma is a common lung condition that causes occasional breathing problems. The main symptoms of asthma include wheezing and shortness of breath. There may be times when the symptoms get better and times when they get worse.
What causes asthma?
What causes asthma is different to what triggers asthma: The causes are the underlying reasons why someone gets asthma in the first place. If there's asthma, eczema, hay fever or other allergies in your family it makes asthma more likely. If you have asthma yourself, your child is much more likely to have asthma too, particularly if both parents have asthma. There's slightly more chance of asthma being passed on by the mother than the father. Children with allergies are more likely to develop asthma, they are said to be atopic. This is usually something that runs in families, and a child who has eczema and a family history of allergies is more likely to develop asthma than other children. Research has shown that smoking during pregnancy and smoking around a baby or child significantly increases the risk of a child developing asthma or other breathing conditions. Children who are born prematurely (before 37 weeks) are also more at risk of asthma, especially if they needed a ventilator after birth to help them breathe.
Bronchiolitis
Bronchiolitis is caused by a virus, and usually affects babies and young children under two years old. It leads to swelling in the lungs and airways. This makes it harder to breathe, and your child will cough and wheeze. If your child has had bronchiolitis a lot, they could be more at risk of developing asthma as they get older. Your baby will be more at risk of bronchiolitis if you smoke.
Triggers factors are things that can make asthma symptoms worse.
Exposure to triggers at work Occupational asthma is a type of asthma caused by certain things found in the workplace, such as chemicals or dust from flour or wood. If you haven't had asthma before and then get it because of the work you do, and if your symptoms improve when you're not at work, you probably have occupational asthma. (Occupational asthma is a common cause of adult onset asthma).
Female hormones
Hormones can play a part in triggering late onset asthma and some women first develop asthma during or after the menopause. Environmental Pollution plays a part in causing asthma. Environmental asthma including traffic fumes and chemicals from power plants, can make asthma symptoms worse and may play a part in causing asthma. Studies suggest that children living near very busy roads are more likely to develop asthma.
Symptoms of asthma
The most common symptoms of asthma include:
- Cough
- Wheezing
- Breathlessness
- Chest tightness
You don't need to have all these symptoms to have asthma. They may only happen when you react to a trigger like pollen, dust, cigarette smoke, cold air or pets. The only way to find out for sure if it's asthma is to go to the doctor. If it's not asthma, your symptoms could be a sign of something else, such as chest infection or a bad cold, so it's worth getting checked out.
Cough
You may notice your cough keeps coming back and/or is accompanied by a wheezing sound. Coughing is often worse at night or early in the morning.
Wheezing
Wheezing is a high-pitched whistling noise coming from your airways, mostly when you breathe out. Some people feel their asthma has gone because their wheeze comes and goes, or is hard to hear, but you can still have asthma even without the wheezing noises, so don't put off seeing your doctor.
Breathlessness
You might get short of breath even after light or moderate activity. This can come on quickly or gradually. Breathlessness can also mean trouble breathing out, as well as in, and having to concentrate to regulate your breathing. You may even struggle to talk, eat or sleep.
Chest tightness
Chest tightness is often described as having a heavy weight on the chest, a bit like being crushed by an elephant. It may feel like a dull ache, or a sharp stabbing in the chest. It can make it difficult to take a deep intake of breath.
Types of asthma
Allergic asthma
Allergic (or atopic) asthma is asthma that's triggered by allergens like pollen, pets and dust mites. About 80% of people with allergic asthma have a related condition like hay fever, eczema or food allergies. If you have allergic asthma your doctor is likely to prescribe a preventer inhaler to take every day and a reliever inhaler to use when you have asthma symptoms.
Seasonal' asthma
Some people have asthma that only flares up at certain times of the year, such as during hay fever season, or when it's cold. While asthma is always a long-term condition, it's possible to be symptom-free when your triggers aren't around. If you've been diagnosed with seasonal asthma or think you have it, speak to your GP or asthma nurse about the best ways to manage it.
Occupational asthma
Occupational asthma is asthma that's caused directly by the work you do. You might have occupational asthma if your asthma symptoms started as an adult and your asthma symptoms improve on the days you're not at work. Occupational asthma is usually a type of allergic asthma. For example, if you work in a bakery you might be allergic to flour dust, or if you work in healthcare, the dust from latex gloves could trigger symptoms.
Non-allergic asthma
Non-allergic asthma, or non-atopic asthma, is a type of asthma that isn't related to an allergy trigger like pollen or dust, and is less common than allergic asthma. The causes are not well understood, but it often develops later in life, and can be more severe.
Difficult asthma
Some people with asthma have what's known as difficult asthma. Sometimes asthma is difficult to manage because of other health issues you have, including allergies or because you have trouble remembering to take your preventer medicine. The signs of difficult asthma are: Asthma symptoms that don't go away, even with high doses of asthma medicines and add on treatments. Needing to use your reliever inhaler three or more times a week. One of the warning signs of an asthma attack.
Frequent asthma attacks
If you have difficult to control asthma you should be able to find a combination of asthma medicines that work for you, with the support of your GP or asthma nurse. You might need to see an asthma specialist to work out why your asthma is difficult to control, and look at different treatments.
Severe asthma
About 4% of people with asthma have what's known as severe asthma. Severe asthma is diagnosed in a specialist asthma clinic. You're more likely to be diagnosed with severe asthma if:
1.You've had more than two asthma attacks in the past year.
2.You have ongoing symptoms even though you've been taking higher doses of inhaled steroids, and have tried a long -acting bronchodilator or a preventer tablet (LTRA).
3.You're using your blue reliever inhaler three or more times a week.
4. You're using your blue reliever inhaler three or more times a week.
Adult onset asthma
Asthma often starts in childhood, but some people are diagnosed with asthma for the first time when they become an adult. This is known as adult onset, or late onset, asthma. Some of the possible causes of adult onset asthma are:
- Occupational asthma, this accounts for 9-15% of adult onset asthma.
- Smoking and second-hand smoking.
- Female hormones these can be linked to adult onset asthma
- Stressful life events.
Childhood asthma
Asthma affects around 1.1 million children in the UK. Some children diagnosed with asthma find it improves or disappears completely as they get older. This is known as childhood asthma. Bear in mind, though, that it can return later in life, especially if it's moderate or severe rather than mild.
Asthma treatments
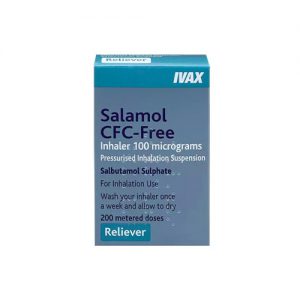
How do reliever inhalers help asthma?
When you have an asthma attack your blue reliever inhaler gets the medicine straight to your lungs, so it can quickly relax the muscles surrounding your airways. The airways can then open more widely, making it easier to breathe again. You should feel a difference to your breathing within a few minutes.
Who needs a reliever inhaler?
Anyone diagnosed with asthma will be prescribed a reliever inhaler, including children under five with suspected asthma. This is to make sure you can relieve asthma symptoms quickly when they come on.
Is a reliever inhaler all you need?
If you only have very mild symptoms, for example if you come into contact with a known trigger, your doctor may prescribe you just a reliever inhaler to use when you get symptoms. But if you notice you're using your reliever inhaler three or more times a week, or you're getting symptoms most weeks, speak with one of our doctors about getting a preventer inhaler too.
What kinds of reliever inhalers are there?
Usually blue, short-acting reliever inhalers contain medicine that relaxes the airways and makes it easier for you to breathe. Metered dose inhalers (MDIs) give the medicine in a spray form (aerosol), for example Ventolin, Airomir and Salamol. Breath actuated inhalers (BAIs), such as Easi-breathe, Airmax, and Autohaler, automatically release a spray of medicine when you begin to inhale. Dry powder inhalers (DPIs), such as an Accuhaler, give the medicine in a dry powder instead of a spray.
When do I need to take my reliever inhaler?
Use your reliever inhaler as soon as you notice asthma symptoms. It can help get your asthma back under control and prevent an asthma attack. If your asthma is triggered by exercise, your doctor may suggest you take your reliever inhaler 20 minutes before you start exercising as this can prevent symptoms coming on. If exercise frequently triggers symptoms for you though, it's worth making an appointment to have an asthma review with your own GP. Asthma symptoms brought on by any kind of exercise can be a sign that your asthma is not well managed. If you need to take your reliever three or more times a week it could be a sign that your asthma isn't well controlled.
What are the possible side effects of reliever inhalers?
Relievers are a safe and effective medicine and have very few side effects. Some people may experience the following side effects after taking a few puffs of their reliever inhaler:
Their heart beats faster for a short while.
Their muscles shake slightly (These usually pass within a few minutes or a few hours at most and are not dangerous).
If you think you've collected more than 12 prescriptions for your reliever inhaler in a year, or you get through more than one inhaler in a month, see your GP or asthma nurse. It could be that your asthma's not well managed and you're at higher risk of an asthma attack). If you have a preventer inhaler and are using it in the right way as prescribed, but you're still having asthma symptoms, you might also need a long-acting reliever inhaler. It's really important to understand that you need to use your long-acting reliever inhaler alongside a preventer, and not on its own.
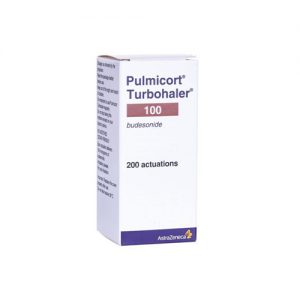
How do preventer inhalers help asthma?
An asthma preventer inhaler prevents inflammation and swelling in your airways. It helps the medicine get right into your airways so it can get to work where it's needed. If you use your preventer inhaler every day as prescribed, using a good inhaler technique, your airways will be less sensitive. This means you'll be less likely to react to your usual asthma triggers. As your preventer inhaler helps stop symptoms coming on in the first place, you may notice you don't need to use your reliever inhaler as much. In order to get the full benefits, you need to take your preventer inhaler every day as prescribed (usually morning and evening) even when you're feeling well. This is because the protective effect of the preventer inhaler builds up over time. There are several different types of preventer inhaler. They all contain a low dose of steroid medicine to reduce inflammation. The steroids used to treat asthma are called corticosteroids. These are a copy of those produced naturally in our bodies. They are completely different to the anabolic steroids associated with bodybuilders and athletes. Preventer inhalers are often brown, they include:
- Metered dose inhalers (MDIs) which give the medicine in a spray form (aerosol). This is the one you often use with a spacer.
-Breath actuated inhalers (BAIs) which automatically release a spray of medicine when you begin to inhale (breathe in).
-Dry powder inhalers (DPIs) which give the medicine in a dry powder instead of a spray.
Does everyone with asthma need a preventer inhaler?
There are very few people who only need a reliever inhaler for when they get symptoms. Most people with asthma benefit from a regular preventer inhaler taken every day to prevent symptoms coming on. This is because preventer medicine, taken as prescribed, builds up your asthma protection over time and helps prevent asthma symptoms.
What benefits can I expect from my preventer?
If you take your preventer inhaler as prescribed, you'll soon start to notice the benefits. For example, you might notice:
- You're less sensitive to your triggers such as cigarette smoke. and colds and flu, because your airways are less inflamed.
- You're able to climb stairs or walk up hills more easily.
- You're sleeping better, and not coughing at night.
- You or your child need less time off work or school.
- You are more able to take part in exercise and family activities.
You won't notice these improvements straight away. But if you keep taking your preventer inhaler as prescribed, and continue to take it even if you feel well, all these benefits could start to feel just part of every-day life. Using a preventer inhaler every day as prescribed makes your airways less likely to react to any triggers you come across. Your preventer inhaler contains a dose of steroid medicine which you breathe in. It controls the inflammation and swelling in your airways and makes them less sensitive to your triggers.
Will you still need to use a reliever as well as a preventer?
If you're prescribed a preventer inhaler, it doesn't mean you should stop carrying your blue reliever inhaler wherever you go. Although they have different jobs, you need both a preventer and a reliever to control your asthma. A preventer inhaler prevents inflammation and sensitivity in your airways over time. This means if you take your preventer inhaler every day as prescribed, you're less likely to react to triggers and get asthma symptoms such as breathlessness. A good routine of taking your preventer inhaler can help cut your risk of an asthma attack. A reliever inhaler relieves symptoms when they come on. It acts quickly when you have an asthma attack but it doesn't do anything about the inflammation building up in your airways.
What are the possible side effects of preventer inhalers?
Most of us have some concerns about possible side effects from the medicines we take. But recent research shows that the chances of side effects from taking a low dose of inhaled preventer medicine are very small. Using your preventer inhaler every day as prescribed, means you're less likely to need your reliever inhaler, or a prescription of oral steroid tablets with higher doses of steroids. Some of the more common side effects are:
- A sore throat
- A hoarse voice
- A mouth infection called thrush.
You can avoid these side effects by making sure your medicine gets straight to your lungs and doesn't stay in your mouth and throat, or get absorbed into the rest of the body. You can do this by:
- Using a spacer with your MDI inhaler
- Using good inhaler technique (you can ask your GP or asthma nurse to check your inhaler technique at your asthma reviews)
- Rinsing your mouth and spitting out
Are there preventer inhalers without steroids?
Some people with asthma are prescribed preventer inhalers that don't contain steroids, such as sodium cromoglicate and nedocromil sodium. But they are not the best option for most people. They're sometimes prescribed for people who don't respond well to steroid inhalers and are not getting the usual benefits from them.
Non-steroid inhalers are not as effective as steroid preventer inhalers at preventing inflammation in the airways. And they need to be taken more often, up to three or four times a day on a regular basis to have an effect.
Steroid tablets for asthma:
Steroid tablets also come in a soluble or liquid form. They contain a higher dose of steroids than a preventer inhaler. For adults, steroid tablets are usually prescribed for at least five days. For children, steroid tablets are usually prescribed for at least three days. If you need a longer course of steroid tablets, your GP or asthma nurse will make sure these are prescribed at the lowest possible dose. You may need to take them for weeks or a few months at a time, depending on the number of steroid tablets you're prescribed, or how long it takes you to fully recover.
Most people who take a short course of oral steroids won't experience significant side effects. You're more likely to notice side effects if you're on a high dose. Although the dose of steroid going into your body is higher if you're taking them in tablet form, any side effects like stomach upset, increased appetite, and mood swings are usually temporary and will stop once the course of tablets has finished.
Additional Asthma treatment For most people, taking a preventer medicine every day and occasionally using a reliever inhaler is enough to manage their asthma. But sometimes people need 'add-on' asthma treatments too. There are several different medicines that fall into this category and they work in various ways, alongside your inhalers, to help you manage your asthma. Examples of add-on treatments for asthma include:
- Leukotriene receptor antagonists (LTRA)
- Theophylline
- Long-acting bronchodilators
LTRA's
These are medicines that are sometimes called 'preventer' tablets, but unlike your preventer inhaler, they don't contain steroids. They work by blocking one of the chemicals that is released when you come into contact with an asthma trigger. They may be particularly effective if your asthma is triggered by exercise or allergies.
- Theophylline
Theophylline works by relaxing the muscles that surround the airways, making it easier to breathe. It's usually prescribed as a tablet that you take twice a day. If your doctor prescribes this medicine, you'll need regular blood tests to check the levels in your body are neither too high nor too low.
Long acting bronchodilators There are three different types of long-acting bronchodilators, long-acting beta agonists (LABA) and long-acting muscarinic receptor antagonists (LAMA). Theophylline is also a long-acting bronchodilator. Long-acting bronchodilators keep your airways opened up by relaxing the muscles around them. This helps you breathe more easily.


We’re here to help.
Our friendly team is available to help Monday to Friday 9:00am - 5:00pm.
If you need urgent assistance, do not use this service. Call 111, or in an emergency call 999.